Is that a knot in my muscle?
54 year old Barbara has pain extending across the top of the shoulders, frequently extending into the neck. Is it a muscle? Is it a trapped nerve? Or is there something more complex going on? Why didn’t it hurt six months ago?
Surely, the muscles are tight?
They may actually be a bit wound up actually, especially with a little bit of stress in your life. Most of us have experienced a rush of adrenaline in the work place, at home or even crossing the road. Adrenaline is great; it prepares your body to get moving by increasing your heart rate and your breathing so you can send more oxygen to your muscles. The free-floating adrenaline also binds to your muscle spindles, increasing the resting tension so your muscles can burst into action.
Most of the time though, we’re left not bursting into action but taking a deep breath and getting on with not moving.
But is all that tension going to make a knot?
One study specifically found there is no clear evidence of a strong relationship between increased electrical activity of muscles and the development of musculoskeletal disorders (2). Keep in mind this was one study, and the definition of a musculoskeletal disorder might not include Barbara and her sore muscles across the top of her shoulders.
I can definitely feel a knot in there.
There is zero consensus about what that hard lump in the muscle actually is and ‘knot’ seems like a fairly innocuous word to all those other than knitters and sailors. And just like knots in the real world, most are amenable to unwinding given the right intervention.
Bio (Body) Psycho (Brain) Social (Environment/Interaction)
Like many things in the body and pain, the pathophysiological mechanisms remain unclear. We are always more than the sum of our parts and if we look at the risk factors above, you need to find out whether Barbara has stress in the workplace, disappointment in her job, her relationship, whether she has a cold, whether her dog just died and she’s stopped walking, whether her children left her with five grandchildren on the weekend? And then what is her ability to control any or all of these aspects of her professional and personal life?
See the problem? This is why a medical history is important, why Osteopaths ask a lot of questions, why we need to spend more than seven minutes with you to grasp how to help you out of pain. We need to find out what’s tipped you from not even noticing that you’re a bit tight, to not being able to tolerate your shoulder discomfort a moment longer.
Hopefully, it’s as simple as softening off the muscles, turning a computer to a better angle, taking some micro breaks in the workplace and heading out for a daily walk.
Let’s get back to Barbara...
Step One:
take a slow deep breath
drop your shoulders
release the tension
Step Two:
get up from your desk occasionally
wave your arms around or run them quickly on the spot for ten seconds
smile at your colleagues and let them know you’re not crazy
Step Three:
Find some daily exercise that you love
Step Four:
Advise your children you can no longer care for all five grandchildren at once for an entire weekend.
References:
Ratey, John J.,Hagerman, Eric. (2008) Spark :the revolutionary new science of exercise and the brain. New York : Little, Brown,
Westad C, Westgaard RH, De Luca CJ. J Physiol. 2003 Oct 15;552(Pt 2):645-56. Motor unit recruitment and derecruitment induced by brief increase in contraction amplitude of the human trapezius muscle.
Morning, I'm Broken!
We all know we feel better physically, emotionally and psychologically if we’ve taken the time to exercise in the morning but how do we reduce the general ache and stiffness that many of us feel before we even get out of bed?
The main thing people consult an osteopath for is pain. Pain in their low back, between their shoulder blades and in their neck.
But a frequent complaint in practice is people reporting a general feeling of stiffness or ache in all sorts of places when they try to leave their beds of a morning. So while the good news is you aren’t woken with pain in the night, the moans and groans start when you haul yourself out of bed. And it can be enough to wake your partner, or the dog.
Is there any research on this?
There was nothing focused in the literature about whether stiffness improves with exercise, and certainly nothing as specific as morning stiffness. Although this may be because no one asked the question in an original study (i.e. it wasn’t set as a specific outcome for the population being studied).
An educated guess…
Waking with stiffness would be due mostly to your body trying to adapt to new behaviours or resting postures you’d get out of given the chance if you were awake.
Examples of the types of things that might cause stiffness in your neck:
Stomach sleeping
Bingeing on Netflix in bed with a laptop
Long long hours at a computer
Long drives on straight roads
Examples of the types of things that might cause stiffness in your low back:
See above
Examples of the types of things that might cause stiffness in your feet and achilles:
Standing for long periods (cooking, ironing, gallery walking)
New exercises or an increase to new exercises (skipping, golfing, new shoes)
Or just good old DOMS the day or two after a workout at the gym
What exactly will you be mobilising?
There is no exactly about it….you’ll be mobilising nerves, muscles, tubes, connective tissue, all manner of fluids including sparking up your brain juices.
A word of caution in the mornings.
Your nervous system is a bit protective of itself when we first wake up, as anyone who has ever done yoga before 6am will attest. That burning tightness behind your knees is not your hamstrings it’s actually your sciatic nerve letting you know it does not appreciate being pulled quite so aggressively before the sun has even risen.
Give it a fortnight.
It might take a while to tell if your body is going to love a new regime but in the meantime you can reward your mornings with these mobilisations:
ACHILLES and FEET stiff when you stand on them in the mornings?
Prancing with straight legs
Heel to toe
Holding onto the door frame squat
If your low back stiff in the mornings?
Try this series of movements:
LB twist
Knees to chest
Cat/Camel
Child Pose with Lateral Flexion
UPPER BACK and NECK stiffness in the mornings?
Sidelying bow and arrow
Neck slider/shoulder shrugs
All our mobilisations will be available on our BLOG this month.
So make yourself a morning routine that suits you.
Share these tips and tricks to put some spring in someone else’s step this August.
HOW LONG UNTIL THIS STOPS HURTING?
Not all pain is caused by tissue damage but there are many occasions when an ‘event' has caused someone to present with pain. Pulling off a tight and sweaty crop top, lifting a heavy pot plant on a weekend clean-out, twisting an ankle during a netball match or landing awkwardly while trying to double bounce your kids on the trampoline.
Four weeks ago, a lovely mid-50s patient kicked a heavy box (that wasn't there before) on a night time bathroom break. She had an x-ray the next day and there was no indication of a fracture and now she is presenting with pain in her toe joint one month later. She is worried the toe may be fractured and the x-ray missed it and now her pain seems to expanding into other areas of her foot.
As students we all learn about how long a tissue injury may take to heal. But this information is infrequently passed on to the patients and I don't think we should underestimate the benefit in learning how long something might take to feel better. It is one of the active ingredients in therapeutic care that we can provide to patients with pain, along with reassurance. Sometimes people don't want to hear that healing and resolution will take 'time' but I'm afraid that's one of the first things we need to accept.
As an absolute minimum these are some common timelines for Tissue Healing:
Muscle Tear: between 2-12 weeks depending on the severity
Acute Tendinopathy: 4+ weeks
Degenerative Tendinopathy: 8+ weeks
Ligament: Between 2-12 weeks depending on the severity (and 12+ weeks if you've had surgical repair)
Internal Disc Derangement: 8+ weeks depending on severity and location
Bone fracture: 8+ weeks (depending on severity)
Bone bruising: 8+ weeks
Most Cartilage injuries: 4+ weeks
Bursa: 2-6 weeks (or on and on and on) depending on severity
Things that will impact tissue healing times (for better or for worse):
- Underlying bony change (age related or previous injury)
- Anti-inflammatories
- Progressing exercise too fast
- No exercise
- Sitting on your butt 9 hours per day
- Eating great or crap food
- Drinking alcohol
- Drinking caffeine
- Drinking sugary drinks
- Age
- Occupation
- Values (have you got a big game to play?)
- Beliefs (your father thinks you're weak)
- Sleep or lack of...
- Stress
Keep in mind we are talking about tissue healing times here and this is something completely different from whether you are experiencing pain or whether you have terrific or terrible function (read this entry here for more on the complexity of pain).
Back to our lovely mid-50s lady with sore toe. Potentially, when she kicked her toe into the heavy box, she didn't fracture the long bone but compressed the ends of two bones into each other essentially bruising the bone. This bruised bone takes a lot longer to heal than a bruise to the skin and the soft tissue just below it and this means it may also hurt for longer.
Finally, walking around with that sore toe can mean you may start to move through your foot differently avoiding the sore joint. You might weight bear more on the foot that doesn't hurt. Your whole body is invested in reducing the pain in your foot and so adapts to give your poor old toe the time and space to heal and recover. Learning about this can help your anxiety around your sore toe and even reduce pain levels. And of course manual and physical therapy provided by the Osteopaths at Fairfield Osteopathic Clinic can certainly diagnose, treat and provide education and advice to help reduce your pain and your anxiety about 'how long until this stops hurting'.
To make an appointment book online or call 9489 0981
Blocked Drains?
Manual Lymphatic Drainage
Manual Lymphatic Drainage (MLD) is an interesting example of a specific massage technique. It is purported to reduce swelling and is used to treat patients suffering from lymphoedema, or swelling of one or more limbs.
Lymphoedema can occur due to compromise or partial failure of the lymphatic system.
WHAT IS THE LYMPHATIC SYSTEM?
The lymphatic system is a complex network of tiny channels throughout the entire body. It’s primary function is drainage, circulation and filtration of fluid throughout the body and it also plays a significant role in immune response. In general, movement of the body creates the “pumping action” required to propel lymphatic fluid through this system.
Occasionally, underlying factors reduce the ability of the body to remove fluid. Factors including medication, disease, pregnancy, excessive weight or trauma. It is also frequently seen as a complication of mastectomy after lymph node removal or other surgical procedures.
WHAT HAPPENS IN AN MLD TREATMENT
MLD is a specialised technique in some practitioners’ tool belts. It is a fairly technical process and practiced by no more than a few hundred therapists in Australia. Petra Miliankos, the Myotherapist at Fairfield Osteopathic Clinic, outlines her approach to MLD:
“When the body gets into the position of not being able to clear fluid on it’s own, an external force (in this case a qualified human) can help remove the barriers to fluid removal.
When you learn MLD you study the movement of fluid along the channels from the tips of the toes and fingers in toward the main ducts in the pelvis and torso. By applying precise, gentle, rhythmic strokes along lymphatic pathways you can help move fluid through the channels.”
WHAT DOES THE RESEARCH SAY?
STUDY OF FOUR WEEKS OF MLD TREATMENT
One study (1) followed short-term MLD (over four weeks) and showed it can ameliorate chronic venous insufficiency severity, oedema, symptoms (fatigue and heaviness), pain and quality of life. Interestingly, the changes you might normally measure like range of motion, leg volume and strength showed no improvement. Quality of life measurements are extremely important, especially for the patient, and are often overlooked in studies.
But wait - doesn’t everyone feels better for a short time after a hands on treatment? True, however the patients in this study reported continued improvement four weeks after the last treatment. Petra said this confirms her experience:
“Anecdotally, clients report feeling better despite not meeting a drastic reduction in limb size. But this perceptual shift can be an important step towards self-management. A recent example is after only three treatments one of my clients felt significantly more mobile and confident enough to pursue an increase in exercise. She is now swimming twice a week at Northcote Pool. I’d say that’s a very positive outcome.”
FURTHER RESEARCH?
A 2015 literature review (2) confirmed the mixed outcomes in the evidence for MLD. There remains no gold standard protocols for the treatment of lymphoedema, so an individualised and clinically reasoned approach, like MLD, remains a valid option.
If you would like to speak to Petra to discuss whether MLD might benefit you, please call the clinic on 03 9489 0981 or book online.
(1) Dos Santos Crisotomo, R.S., Costa, D.S.A., de Luz Belo Martins, C., Fernandes, T.I.R., Armada-da-Silva, P.A. (2015). Influence of Manual Lymphatic Drainage on Health-Related Quality of Life and Symptoms of Chronic Venous Insufficiency: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, 96(2); 283-291
(2) Finnane, A., Janda, M., & Hayes, S.C. (2015). Review of the evidence of lymphedema treatment effect. American Journal of Physical Medicine & Rehabilitation, 94(6): 483-498
Five tips for a better night's sleep.
Sleep is a tricky topic. How many hours should we get? Seven, eight or nine? What has been the impact of television/screens/ipads? Should we sleep more like our ancestors in two big chunks (Bi-modal sleep)?
The overwhelming response from most people would be that they'd really just like a bit more of it.
Here's my top five tips to get a better night's sleep:
1. Stop unhealthy habits before bed
Finish eating or drinking at least two hours before you try to lie down.
Get off that computer or off the couch at least one hour before bed - seriously.
Check any nighttime medications* don't have caffeine in them.
2. Clear your bedroom of unhelpful items (make a checklist)
Get a blackout curtain if a street light shines in (it's not just for toddlers).
Is your room too warm or too cold?
Get rid of your shining alarm clock. No one needs to see the time in neon.
Turn off your mobile phone. I mean it.
Children and pets are warm, nurturing creatures but they don't always need to share the bed with you. We often get shoved into a cold corner of the bed to accommodate them. Restore your boundaries.
Is your mattress more than 8-10 years old? It might be time for an upgrade.
Do you love your pillow? (see my post on pillows)
Covers too heavy or restrictive?
Spouse or partner that is restless, noisy, or generates too much heat - um, acceptance?
Some medical conditions❡ interfere with sleep.
3. Do you love a daytime nap?
Do not daytime nap for more than 45 minutes
No napping after 3 pm
4. Exercise
A few surprises. A 2010 (1) study found people with no previous sleep difficulties slept better the night following exercise. But for people who had been diagnosed with insomnia, a fairly comprehensive study from 2013 (2) found people had to exercise daily and consistently for up to four months before there was a measurable benefit.
Put simply:
Consistently do a bit more physical activity during the day.
Expose yourself to bright light on waking – tell your body it's daytime.
Expose yourself to bright light in the afternoon to keep your body awake longer.
5. Consistency of sleep habits
Wake up at the same time every day - almost the hardest one to implement for anyone, especially an insomniac.
Develop a flexible before bed routine. It might include a warm shower or bath, meditation or a calming book.
In-bed routines - breathing techniques, progressive muscle relaxations (that's a whole other BLOG)
Reduce fluid consumption in the evening to avoid the need to wee all night.
(1) Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. Oct 2010; 11 (9): 934-940. Kathryn J. Reid, PhD, Kelly Glazer Baron, PhD, Brandon Lu, MD, Erik Naylor, PhD, Lisa Wolfe, MD, and Phyllis C. Zee, MD, PhD
(2) J Clin Sleep Med. 2013 Aug 15;9(8):819-24. Exercise to improve sleep in insomnia: exploration of the bidirectional effects. Baron KG1, Reid KJ, Zee PC.
* Some medications that can interfere with sleep:
- Antihistamines: Benadryl (daytime drowsiness)
- Sympathomimetic Amines: bronchodilators and decongestants
- Antihypertensives and Beta blockers: Clonidine, Aldomet, Reserpine (daytime drowsiness)
- Steroids: Prednisone, dexamethasone
- Thyroid medications:
- Anti-epileptics and antipsychotics (daytime drowsiness)
- Parkinson medications: (daytime drowsiness)
- Stimulants for ADHD
- Anticholinesterase drugs for Alzheimer's
- Antidepressants: Prozac, Fluoxetine
- Analgesics: opiates, Tramadol, Ultram
- Chemotherapeutics: (nausea and vomiting)
- Diuretics: (frequency at night)
❡ Some medical conditions that can interfere with sleep:
- Respiratory disorders
- Cardiovascular disorders
- Gastrointestinal disorders
- Musculoskeletal pain and dysfunction (Book Online)
- Diabetes
- Renal disorders
- Prostate problems and small bladder causing urinary frequency
- Cancer
- Dementia
- Dental disorders
- Restless leg syndrome or Periodic Limb Movement Disorder (PLMD)
- Fibromyalgia (alpha wave intrusion)
NOTE: People who do shift work have special challenges as they consistently interrupt their diurnal rhythms. It is outside the scope of this post.
"Them bones, them bones, them dry bones"
by Mark Cooper
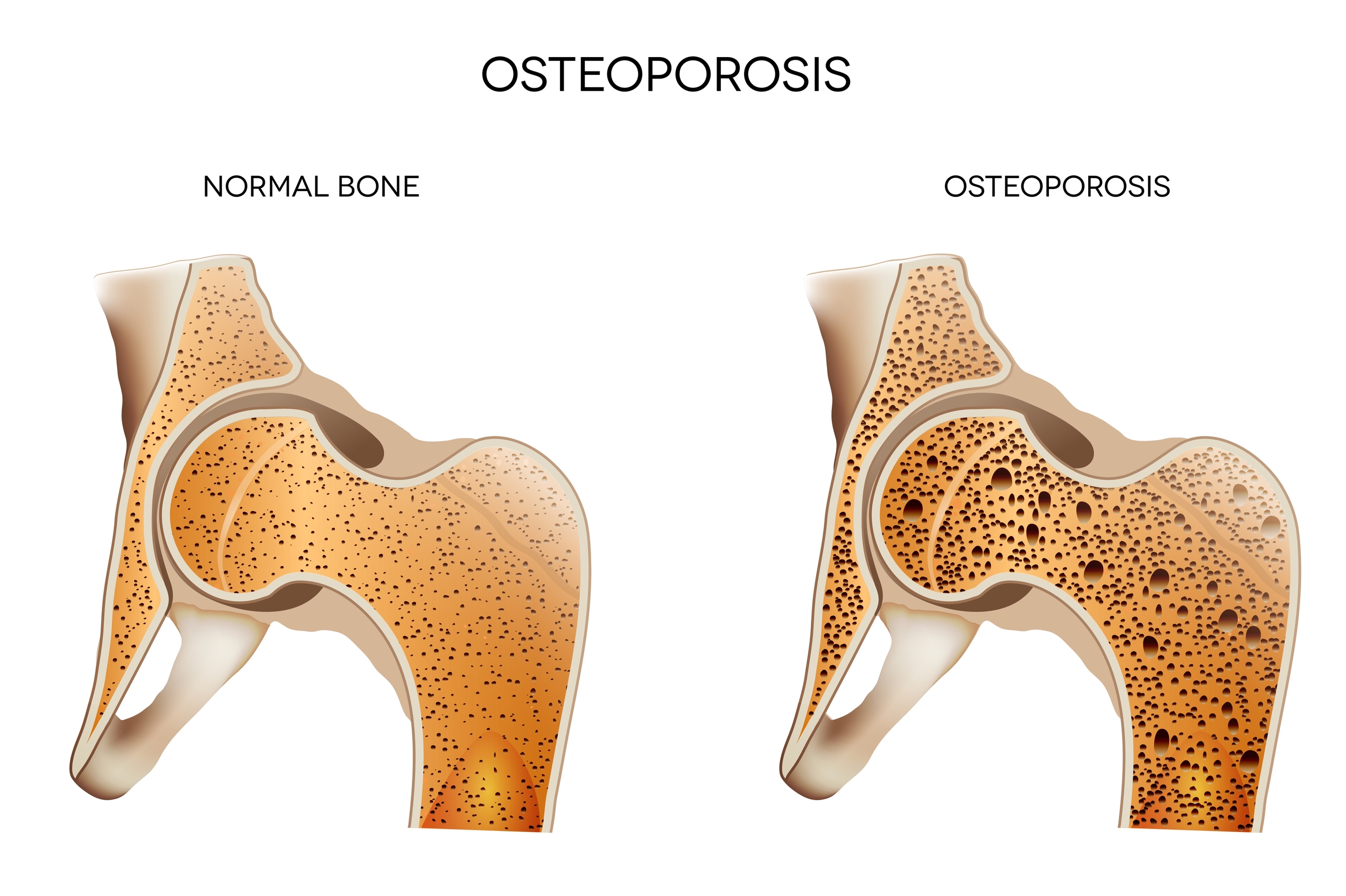
Osteoporosis
I recently sat in on a Webinar entitled "Osteoporosis Update" put on by Arthritis and Osteoporosis Victoria. It was not the most enthralling topic (or speaker) but the take home message was absolute. In an ageing population osteoporosis has become a significant issue.
For the uninitiated, osteoporosis is the process when bones lose their strength and density. When this happens they become fragile, brittle and weak and are much more prone to fracture. Sounds bad doesn't it. Well the good news is that osteoporosis for the most part is preventable (this may not be the case if there is pathology at play or genetic predisposition to osteoporosis).
The 1,2,3 punch - Vitamin D, Calcium and Exercise
The key to prevention is calcium, Vitamin D and weight bearing exercise. It's a winning combination. Calcium is best sourced from food but there are many supplements on the market.
Vitamin D is what you get when sun and skin combine. This is a little tricky as too much sun can be bad for you so there are some guidelines for adequate sun exposure which are specific to your region in Australia or the world, even sunny Melbourne.
In the height of a Melbourne Summer: 6-8mins of sun exposure between 10am and 2pm.
In Winter: It is more like 30-50mins between the hours of 10am and 2pm.
Walking is just not enough
We have become far too sedentary in our cushy western lifestyle and we all need to work a bit harder to have healthier bones. The National Osteoporosis Foundation (US) has some good guidelines on weight bearing and muscle strengthening exercise for healthy strong bones. (Always consult your health care professional before embarking on an exercise program.)
Some good examples of high impact weight bearing exercise are :
- dancing
- jogging
- aerobics
- hiking
- stair climbing
- tennis
Low impact exercise can be equally beneficial depending on the individuals situation and their relevant bone density:
- eliptical trainers
- low impact aerobics
- fast walking (no lazy Sunday strolls)
- aqua aerobics
Get pushy
Building muscle requires pushing some heavy things around. This can be done at the gym or any type of resistance training. Equally important for muscle building is how you move when you build that muscle. Doing balance exercises, functional movement exercises (e.g. squats, lunges) goes a long way to improving your overall range of movement and your ability to perform the muscle strengthening tasks. The more exercise the merrier, your bones and muscles will thank you.
So in combination with the Vitamin D and Caclium and and active lifestyle go forth and multiply your bone cells. That is our prescription for a healthier you.
1. "Osteoporosis Update" - Webinar - Osteoporosis and Arthritis Victoria
2. http://nof.org/
Oh my aching back! I must be turning 40.
What is it about getting close to 40 years of age? What was once a simple physical task with zero repercussions can quickly become a serious impediment to general movement for days (sometimes weeks and months) afterwards.
Elastics! You remember - “England, Ireland, Scotland, Wales - Inside, Outside, Inside, On!” Who knew this simple childhood activity could be fraught with danger for the nearly middle-aged. Earlier this year, on the rickety floorboards of our little house in Northcote, I decided to demonstrate to my children the art of elastics, only to find myself nursing a particularly sore low back, bum and leg once the demonstration had concluded. No, I didn’t trip on my ego, or anything 38-year old dad like that. I was just very sore afterwards. The muscles in my lower back and left bum cheek had well and truly gone into spasm. By the way, the Germans have a good phrase for acute low back pain - Hexenshuss (1). This literally means “shot by the witch”. I know I didn’t send my daughter to school at Hogwarts, so I safely ruled out the witch angle. The kids were actually impressed with my Quidditch like agility, until they saw me wince with pain.
The result of my brief foray into an innocent childhood activity resulted in three months of sciatica, or to use the correct terminology radicular pain, associated with inflammation or irritation of one of the nerve roots in my low back. I don’t have X-ray vision but I was pretty sure I had herniated one of my discs. While it definitely got me down, I sucked it up and chose to use this as a learning experience about my body and it’s ability to heal.
Acute low back pain with or without pain that heads into the bum or down the leg (radicular pain) is actually very common. Research dating to 1995 showed that low back pain was the 5th most common cause of visiting a GP (2). These numbers have only increased in the last decade. Most of you out there would think that having a disc herniation must mean bad things for the future? But some recent research debunks this entirely. Not only do you not need to have a disc herniation to experience sciatica, but results show that patients who DO have a disc herniation recover just as well from low back pain and sciatica as those who DO NOT have a disc herniation (3). WOAH!
Lets return to why this happened and what I did about it.
The why is actually not that clear. Doing an activity like elastics when you are 95kg as opposed to 22kg might have a lot to do with it. Aside from weight being a factor, we know from research that age does not necessarily predispose anyone to this happening. What we also know is that the more active, fit and conditioned an individual is when they tackle a physical task there is a decrease in likelihood of physical injury from performing that task. (4)
Well after three months I was back to my old self. The low back pain and sciatic symptoms improved with some osteopathic treatment, but mostly I took an active care approach involving graded exercise and pretty soon I was back to running the streets of Northcote with no pain at all.
I’ve found I do have to be a bit careful when doing something out of the ordinary but why that happens belongs in a totally other BLOG post.
Obviously not all back pain cases are created equal. For instance, when movement continually elicits pain then you might need to check in with your osteopath. It may be a more complicated clinical matter that needs addressing. But don’t worry in most case we can get you back on track and jumping elastics before you can say - Oh My Hexenshuss!
(1) Thanks Paul Ingraham for this little gem - saveyourself.ca
(2) Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Hart LG, Deyo RA, Cherkin DC. Spine (Phila Pa 1976). 1995 Jan 1;20(1):11-9.
(3) Magnetic resonance imaging in follow up assessment of sciatica. el Barzouhi A, Vleggeert-Lankamp CL, Lycklama à Nijeholt GJ, Van der Kallen BF, van den Hout WB, Jacobs WC, Koes BW, Peul WC; Leiden-The Hague Spine Intervention Prognostic Study Group. N Engl J Med. 2013 Mar 14;368(11):999-1007
(4) http://www.sciencedaily.com/releases/2009/02/090220090750.htm