Festivi-Tea Recipes
With Vicki the naturopath concocting the brew, Festivi-Tea was always going to be healthy and pretty.
The ingredients list are all organic and Australian grown:
Spearmint – aids digestion
Rose – Cooling and cleansing
Rosehips – rich in vitamin C and bioflavonoids
Lemon myrtle – anti-bacterial and calming
Hibiscus – supportive of the cardiovascular system
How to enjoy Festivi-Tea
Festivi-Tea makes a refreshing drink as a tea, either hot or cold. It can also be made into a delicious Christmas punch or cocktail.
Flowers by Prickly Pear
To make the tea (hot):
Pour the contents of the bag into a teapot or coffee plunger. Add approximately 2 cups of boiling water and allow to steep for 5-10 minutes.
Pour. Drink.
To make the tea (cold):
As the following recipes are for cooling drinks, brew your tea, allow to cool and then refrigerate for up to 24 hours.
Flowers by Prickly Pear
Christmas Punch
This is a refreshing alternative to the traditional punch, which is full of sugar due to the use of lemonade and ginger ale.
Mix together:
2 cups Festivi-Tea
2 cups apple juice
1 cup soda water
Add lots of ice and sliced summer fruits such as strawberries and nectarine. You can try a different juice or add chopped mint leaves for an extra kick.
Christmas Cocktail - for adults only
Mix together:
2 cups Festivi-Tea
1 bottle of Prosseco (sparkling wine)
Add one punnet of chopped strawberries and enjoy.
Michael Clarke's Back
Anyone who was watching the cricket yesterday would have seen the incident that led to Michael Clarke leaving the field with severe back pain. For the uninitiated Michael Clarke is the captain of the Australian Cricket team. The last week or so may have been, quite probably, the most traumatic and stressful period of his life so far. Recently there was the tragic injury, while batting, and subsequent death of Australian cricketer Philip Hughes. Phil Hughes happened to be a very close friend of Michael Clarke. A sad event all round and our condolences go to family, friends and the cricketing community at large.
I won't presume through this Blog to know exactly what is happening with Michael Clarke's lower back. I've heard it all from the commentators and journalists - disc degeneration, disc prolapses, sprained sacroiliac joints, pars interarticularis fracture - and the list goes on. No doubt he has a team of specialists giving their two cents on what is wrong and what he can do about it. What interests me is how such an innocuous incident could lead to a flare up of a pre-existing complaint.
The previous week Phil Hughes was felled by a bouncer while batting for NSW. Without going into detail it was a tragic and unfortunate accident that ultimately ended his life. Yesterday, while facing up to the Indian pace attack in the first Test Match of the summer Michael Clarke was travelling along quite well. He has recently altered his batting technique to take pressure off his "niggly" low back and hamstrings and it seemed to be working well. The Indian bowler at the time bowled a bouncer at Michael Clarke (which was a pretty ordinary ball putting the batsman under little pressure at all) to which he flinched to instinctively get out of the way. Wham-Oh! His back went into spasm and he was unable to continue.
Michael Clarke was under pressure - emotionally and physically. He was carrying a "niggly" lower back and hamstring problem. Suddenly a bouncer comes at him at 140km/hr and his brain says "ALERT, ALERT!" There is a reflex tensioning of the body and the messages from the brain to the lower back were greatly exaggerated. Here is a perfect storm for aggravating a pre-existing problem. Stress, anxiety and physical duress can all impact on the DANGER signals to the brain and the way the brain interprets that danger. It is quite likely Michael Clarke has not done any further "damage" to his lower back, and honestly I hope he is not being told how "damaged" his lower back is as it does not directly equate to a persons pain experience one iota.
Michael Clarke is an impressive captain to bravely go out and face that red ball under such stress and I'm sure will bounce back and hopefully be better for it. In fact, I think he just got a century.
Referrals from Dr Google
Why Dr Google isn’t always enough.
A colleague of mine in Canberra recently saw a teenage girl whose mother had noticed a curve in her spine. Her mother was worried and took her daughter to her GP. She was diagnosed with a Scoliosis and referred for X-rays. The X-rays suggested the curve was so pronounced she was a candidate for bracing and/or surgery and the GP referred her to Canberra Hospital. Due to the nature of a regional hospital, Canberra didn’t have anyone appropriate to help the girl and sent her away. Unfortunately, they didn’t provide any further referral advice.
As the mother was a client of my colleagues, she asked if she could review her daughter’s situation. My colleague assessed her, read the report, looked at the X-rays and agreed with the findings. Your garden variety Scoliosis* is rarely anything to be concerned about but this girl’s Scoliosis was very pronounced and due to her age, was at risk of progressing with potentially serious side effects. My colleague knew, in this case, her place wasn’t in providing hands-on therapy or exercise advice. The young girl didn’t have any pain. She reassured both the parent and young patient she would look into what the protocol was from this point.
The Mishits
My colleague completed a Google search of her own. The initial hits were private clinics offering exercise therapy from physiotherapists and spinal alignment from chiropractors. Either of these methods, even with the fanciest websites, and expensive treatment programs weren’t offering much for a spinal curve that could impact the long-term health of this young girl. As an Osteopath interested in the evidence behind making decisions in clinic she dug a little deeper and started to search journal articles and systematic reviews about Scoliosis.
Good advice, and therefore opinion, should change as new research enters the fold; exercise, bracing and surgery were all still in the offing but they were used for different grades of Scoliosis. And she was no closer to finding an expert who could help this young girl with her choices.
The Resolution
Many health professionals, especially Osteopaths, often work in isolation. For a whole lot of reasons it can be hard to communicate with other health professionals. It’s called cross-referral.
My colleague rang me to discuss the situation. I followed up her phone call by speaking to a friend who is a paediatrician at the Royal Children’s Hospital in Melbourne. She suggested sending her to a big centre in Sydney to see a paediatric orthopaedic surgeon for assessment and advice. Her advice emphasised consulting a bigger centre as even bona fide specialists are prone to working in isolation. They might have forgotten to keep up with the evidence and then you can be right back where you started.
There are also particular ways to take an X-ray of a Scoliosis that give a more accurate measure of the curve. A big centre will organise this and it may mean this girl is not in as dire situation as her report suggests. That’s worth knowing.
Occasionally, especially when it comes to making decisions about our health, we find ourselves at a loss, and we turn to Google for advice. As magical as Google is, it doesn’t always cough up the best evidence-based advice. There are a lot of people with something to sell, trying to make their living on the WWW.
There are also some amazing people, who have studied a long time and continue to gather the evidence, and question the current dogma in support of what they do. They may not have as much time to construct websites and complete digital marketing strategies that mean they’re ‘top of the pops’ on a Google search. What they do have is more than an opinion. In the case of this young girl, she was best off to navigate the fragile behemoth that is our amazing public health system. My colleague, an Osteopath, has the skills, contacts and strategy to help her navigate the system, interpret the advice and provide reassurance. She will also be there to help rehabilitate her after intervention with movement advice or provide pain relief - should she need it.
My take home point
The health professional you visit, whether it’s your GP, Osteopath, Maternal and Child Health Nurse, Naturopath or Dentist, should be interested in providing advice and treatment based on current best practice, science and research.
Times have changed and will continue to do so. The healthcare/medical sphere is continuing to evolve. As a consumer, it is in your best interest to seek out the professionals that are interested in treating you in this manner because then your healthcare complaint will be managed with the most current information available - NOT ‘this is how we’ve always done it’.
The Osteopaths at Fairfield Osteopathic Clinic are all university trained in their area of expertise. They know their limitations. They have the skills to navigate the healthcare system and will better equip you in your journey. As Osteopaths we also have more time to provide this extra support you require ….. GP’s are VERY busy people.
(1) Epidemiology of adolescent idiopathic scoliosis. Markus Rafael Konieczny, corresponding author Hüsseyin Senyurt, and Rüdiger Krauspe. J Child Orthop. Feb 2013; 7(1): 3–9.
* Very few humans on this planet have ‘perfect’ alignment. Millions of people have Scoliosis (1) - a sideways curvature of the spine - with no undue stress or strain placed on any part of our bony structure, or the muscles and ligaments that attach to it.
Extra information
The Internet is an amazing resource, full of information and misinformation. This is a great link that questions the value of opinion: http://theconversation.com/no-youre-not-entitled-to-your-opinion-9978
Frozen Peas vs Nana's Hot Water Bottle
I know. You just want it to be simple.
Today, I can make it simple for you.
You've got pain (somewhere) and the question running through your mind is, "Should I use heat or ice"?
So........
ICE is for INJURIES. Use it for:
Distracting
Modulating INFLAMMATION after muscle trauma - think sprained ankle or a 'corkie'
Any 'micro' muscle trauma - think big workout at the gym or beefy AFL players braving the Southern Ocean in July
And it's generally used during the first few days - think FIRST AID
Pain relief
Heat is for, well, HEATING. Use it for:
Tight muscles
Relaxing
Softening
Stress relief*
Warming
It's kind of like a cuddle - it's nice for the body and the mind
Pain relief
When the wrong choice can make it worse:
Heat is generally thought to increase blood supply to an area, so if you have a muscle that is inflamed e.g. pulled, torn, etc. then using heat might make it worse.
If you have a tight muscle and it's been that way for quite a long time (but nothing is injured or torn) then chances are you'll make yourself more uncomfortable using ice. It won't cause any damage but a neck in spasm is worse than a tight one.
When the wrong choice doesn't matter a bit:
And did you notice that pain relief is mentioned in both heat and ice. A 2010 study when either a heat or ice pack was given in addition to nurofen, both were deemed equally effective (in a very minor way).
So, if it's 40 degrees outside on a hot Melbourne summer day and you start using a heat pack and realise that it feels wrong (which it no doubt would). Switch and try the ice.
Garra et al. Heat or cold packs for neck and back strain: a randomized controlled trial of efficacy. Academic Emergency Medicine. 2010
* It's therapeutic effect is quite complex (like everything to do with the body and brain) but there is no additional benefit to understanding the neurophysiology behind heat and pain (well, not at the moment).
"Them bones, them bones, them dry bones"
by Mark Cooper
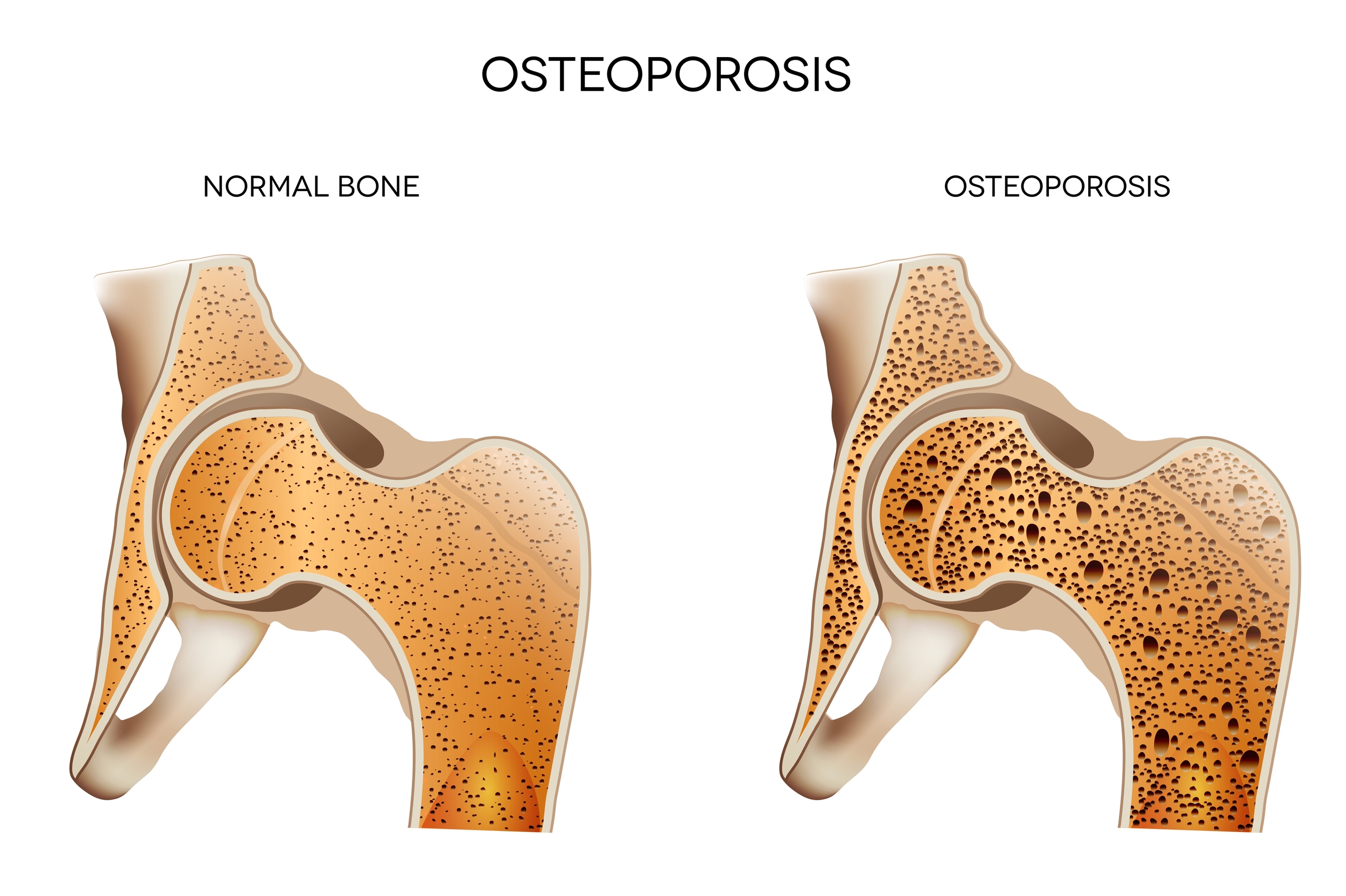
Osteoporosis
I recently sat in on a Webinar entitled "Osteoporosis Update" put on by Arthritis and Osteoporosis Victoria. It was not the most enthralling topic (or speaker) but the take home message was absolute. In an ageing population osteoporosis has become a significant issue.
For the uninitiated, osteoporosis is the process when bones lose their strength and density. When this happens they become fragile, brittle and weak and are much more prone to fracture. Sounds bad doesn't it. Well the good news is that osteoporosis for the most part is preventable (this may not be the case if there is pathology at play or genetic predisposition to osteoporosis).
The 1,2,3 punch - Vitamin D, Calcium and Exercise
The key to prevention is calcium, Vitamin D and weight bearing exercise. It's a winning combination. Calcium is best sourced from food but there are many supplements on the market.
Vitamin D is what you get when sun and skin combine. This is a little tricky as too much sun can be bad for you so there are some guidelines for adequate sun exposure which are specific to your region in Australia or the world, even sunny Melbourne.
In the height of a Melbourne Summer: 6-8mins of sun exposure between 10am and 2pm.
In Winter: It is more like 30-50mins between the hours of 10am and 2pm.
Walking is just not enough
We have become far too sedentary in our cushy western lifestyle and we all need to work a bit harder to have healthier bones. The National Osteoporosis Foundation (US) has some good guidelines on weight bearing and muscle strengthening exercise for healthy strong bones. (Always consult your health care professional before embarking on an exercise program.)
Some good examples of high impact weight bearing exercise are :
- dancing
- jogging
- aerobics
- hiking
- stair climbing
- tennis
Low impact exercise can be equally beneficial depending on the individuals situation and their relevant bone density:
- eliptical trainers
- low impact aerobics
- fast walking (no lazy Sunday strolls)
- aqua aerobics
Get pushy
Building muscle requires pushing some heavy things around. This can be done at the gym or any type of resistance training. Equally important for muscle building is how you move when you build that muscle. Doing balance exercises, functional movement exercises (e.g. squats, lunges) goes a long way to improving your overall range of movement and your ability to perform the muscle strengthening tasks. The more exercise the merrier, your bones and muscles will thank you.
So in combination with the Vitamin D and Caclium and and active lifestyle go forth and multiply your bone cells. That is our prescription for a healthier you.
1. "Osteoporosis Update" - Webinar - Osteoporosis and Arthritis Victoria
2. http://nof.org/
You can't take a picture of your pain.
by Mark Cooper
It may surprise you to know that two out of every three people you meet today walking your local streets of Northcote, Fairfield or Alphington will have some kind of abnormality of their spine, be it bony change, disc bulge or spinal curve, and they will have absolutely NO PAIN!
That's right folks, they are getting on with their inner-north-hipster-cold drip coffee culture lives totally oblivious to the changes in their low backs. I hear you ask "How can this be?"
These changes are, for the most part, a normal process of ageing and the body is very good at adapting. What the research boffins know is that without a doubt MRI, CT scan and X-ray results DO NOT predict the amount of pain you will be in or even that you will experience pain at all.
I outright avoid sending people for scans. There is a time and a place to order them, especially if there are serious indicators, however, there is an ever growing issue regarding the amount of medical imaging being ordered across all facets of health care. But I'll focus on my niche area - LOW BACK PAIN.
A systematic review and meta-analysis (that is the bees knees of research thoroughness) was done on imaging strategies for low back pain in 2009 and published in the Lancet Journal (that's a seriously good place to land your research study). The findings were as follows:
"Lumbar imaging for low back pain without indications of serious underlying conditions DOES NOT (my emphasis) improve clinical outcomes. Therefore, clinicians should refrain from routine, immediate lumbar imaging in patients with acute or subacute low back pain and without features suggesting a serious underlying condition." (1)
Have you heard the one about the man with low back pain who walks into the Osteopath/Chiropractor/Physiotherapists' clinic? From the history and examination there is no indication of anything sinister. Three treatments later with no change to the patient's pain experience, he is starting to get concerned and lose faith in the practitioner's ability to help him. The practitioners ego is taking a battering so they need to bump up their authority with the words "better get a scan" and "this doesn't look good". Low and behold the scan report has some big foreign words in it. Words like osteophytes, foraminal encroachment, decreased lumbar lordosis - could it be any worse? This confirms the patient's fears and they immediately start to feel negative about their prospects of making a full recovery. Their mind starts racing with black cloud scenarios like, "I'm going to have to stop running, I'm only 45 and how am I going to play with my kids?" Crotchety Uncle Brian appears in his mind, fast asleep in his wheelchair at Christmas after his third back surgery, drooling from the mix of codeine and alcohol in his system. Often all the practitioner has to offer is "I told you so - it's bad - you're going to need to see me a lot in the future." The patient is disempowered from every angle.
There are real dangers of associating findings on an X-ray to a patient's experience of pain. Pain is complicated (ouch, there is that word again). It hurts my brain how complex pain is, no wonder patients and practitioners across the board avoid explaining it properly. Pain is a process driven by the brain and negative reinforcement of a patient's pain may be extremely detrimental to their recovery.
Scans can also be used against you in a massive sales pitch from dodgy practitioners. Treatment plans will usually involve 'straightening' your spine with manipulation three times a week for six months and 'oh, could you pay for that up front'. Other practitioners might show you how to strengthen your core in any number of ways - most of them will be expensive and involve you handing all sorts of power over to them.
The best evidence suggests that most cases of serious low back pain resolves within weeks. A bit of reassurance, good advice and pain relief from a competent practitioner might help and leading an active, healthy lifestyle should be the primary prescription going forward.
At Fairfield Osteopathic Clinic we are always cautious when ordering scans for patients. Even when patients present with scans (that we didn't order) we try to use positive language to explain the results and findings, as the pictures of your insides do not reflect the way someone is feeling on the outside. Remember you can't take a picture of your pain.
1. Dr Roger Chou MD, Rongwei Fu PhD , John A Carrino MD, Prof Richard A Deyo MD - The Lancet, Volume 373, Issue 9662, Pages 463 - 472, 7 February 2009
What is the difference between an Osteopath, Physiotherapist and Myotherapist?
written by Mark Cooper
This is one of the most common questions from new patients in my daily practice. People sense I'm not going to laugh at their naivety and out it pops halfway through the first treatment. My answer always errs on the side of caution as I don't really know what happens in other clinics. My answer is occasionally long winded as it's all about Philosophy, Philosophy, Philosophy.
Philosophy is one of those words that sometimes throws people. We know philosophers are intellectuals, thinkers or academics but ultimately, philosophy is just a theory or attitude that acts as a guiding principle for behaviour. That's what separates the individual disciplines, and of course, that's what separates individual practitioners and results in the treatment you'll receive.
I think an example is in order.
George, a 39 year-old office worker, saw the sun shining on the weekend and realised his deck needed some serious maintenance. He bought some Cutek-CD50 deck cleaner and he started in, on his hands and knees, scrubbing the sucker. It took longer than anticipated. His knees were raw but it was his left shoulder that kept him up that night, throbbing uncomfortably into the early hours of the morning. Upon waking, it was heavy, sore and he couldn't lift his arm above his head. He realised thousands of repetitive movements that he had never done before might have resulted in some pain.
He went to work, and by 3pm, he was Googling 'shoulder pain' 'Fairfield' and 'relief'. He wasn't really sure what he needed but it wasn't a footy injury and he winced at the thought of someone massaging it. Google brought up Fairfield Osteopathic Clinic and he remembered his sister saying she'd seen an osteopath and thought they were awesome. Even better, as he considered himself tech savvy, he could book online for that day. Done. His shoulder felt better already.
What happened in the treatment?
He travelled up Station St, Fairfield and found himself in the waiting room. Mark Cooper, shook his hand and in the consultation room Mark took a thorough case history which included much detail about the "deck incident" as well as his previous medical history. George was extremely anxious about his shoulder pain as his neighbour had recently had a shoulder operation for long standing shoulder pain that did not go well. This is where the reassurance of George began.
From that point on George was in good hands. Examination included some orthopaedic tests for his shoulder that were necessary to gather what muscles/joints/soft tissues/nerves were ringing alarm bells. With a diagnosis in-hand George was treated with hands-on techniques that aimed at reducing pain so that George could confidently move his shoulder uninhibited. In short, there was a complete bio (body) psycho (brain) social (environment) approach to George's pain.
George was NOT told there was an imbalance of the strength of his muscles around his upper back and shoulders, or that his spine was out of alignment leading to restriction of the nerves coming from the neck to the shoulder which were now inflamed. Unfortunately, these kinds of poor diagnoses and explanatory models of pain and injury still exist and they don't help George one bit!
What would another practitioner do?
Okay, so what would the physiotherapist have done differently. The question, equally might be, what would an osteopath at another practice in Northcote have done as it might be just as different. Can you sense me stalling?
Physiotherapists may do less hands-on treatment, they historically like heat-packs* and ultrasound, although that's changing. You'll get exercises and advice. They know, like us, that this particular injury will get better on its own, so you don't need much intervention as long as you keep on moving it. Many physiotherapsists (not exclusively) tend to over-complicate some injuries and you might find yourself being referred into Pilates (at their clinic) or buying a theraband for a set protocol of exercises.
A Myotherapist allies itself with remedial massage therapy and focuses on musculo-skeletal health. They will be able to help relieve your pain by working on the muscles around the shoulder. Some have a degree in Allied Health that takes four years, which is as long as physiotherapists train. This doesn't mean their training is similar. Physiotherapists are supported in their education by hospital placements. Osteopaths train for five years, although outside the hospital system.
This is a big, messy discussion that covers diverse debates around contentious topics including clinical reasoning, capabilities and competencies, sandstone universities versus private institutions, vested interest and education as a commodity. The most skilled, educated and compassionate Myotherapist may be more than equal to a complacent Physiotherapist or Osteopath. This is true in a variety of professions.
* Hey, I like heat packs as much as the next person but it's much cheaper to use them at home.
No references today, as this particular BLOG is full of anecdote and opinion.
What Exercise Should I Be Doing?
written by Angie Bruce
Should I be doing Pilates? I’ve been told my core is weak.
I can’t run anymore. I’m worried about my knee pain.
People frequently ask me to tell them what is the perfect exercise. Generally my advice about exercise is very simple. Choose the exercise that you will actually get out of bed and do.
Recognise you might have a competitive spirit, so find a team sport, or use STRAVA to compete online with your friends. You might need others to work with to help keep you motivated, so group exercise is fantastic for that. You might have very limited time, well walking out the door and running might be better. You love swimming but hate what it does to your hair, so it’s probably not worth pursuing.
I used to love cycling but I can’t find the time anymore with kids.
I know I've used this excuse but what better way to show kids that it’s essential to find time for exercise in their own lives. And of course, it’s really good for them too. Psychologists from the University of Illinois at Urbana-Champaign studied how exercise affects the actual shape and function of children's brains. They found that fit children scored better in a series of cognitive challenges (1).
My low back grumbles every time I start back at the gym, so I think I might be damaging it.
If your low back grumbles at the gym, it’s probably just in shock and you might need some advice about how to pace back in. Remember a whole lot of sitting has happened to your body since you stopped moving at twenty-three. An osteopath can provide you with advice and reassure you about how to start back safely in your chosen activity.
Is walking enough?
Apart from a few pockets of the population, like those at risk of osteoporosis, walking is generally enough. Half an hour, four times per week. Spring is in the air, the days are getting longer and it should be enticing to get outside.
I love walking and often listen to podcasts (or silence with noise cancelling headphones but that’s another BLOG) instead of the cars, sirens, helicopters and coffee machines around the streets of Fairfield and Northcote. But I also really like pushing heavy things around and I’m motivated by working out with other humans. So Crossfit has sparked an interest and the trainers at Charge Crossfit are helping me push myself, as I’m not one to do that alone.
The Benefits of Exercise
Exercise should make you feel good, build muscle and improve your cardiovascular system but the benefits are so ridiculously, overwhelmingly good that if I tell you all the benefits, you’ll become skeptical and stop reading (2).
Oh to hell with it, read this:
- Boosts energy (3)
- Controls weight (4)
- Reduces pain (5)
- Improves mood
- Improves sleep
- Decreases anxiety
- Improves coping mechanisms and reduces stress (6)
If you're still not convinced.
I love this youtube video called the 23 and 1/2 hour day.
https://www.youtube.com/watch?v=aUaInS6HIGo
And in answer to whether you should do Pilates. If you enjoy it, do it, but stop worrying about your core. As long as your guts aren’t falling out of your body, then your core is fine.
(1) Chaddock L1, Erickson KI, Prakash RS, VanPatter M, Voss MW, Pontifex MB, Raine LB, Hillman CH, Kramer AF.Dev Neurosci. 2010 Aug;32(3):249-56. doi: 10.1159/000316648. Epub 2010 Aug 6. Basal ganglia volume is associated with aerobic fitness in preadolescent children.
(2) Carlson and Shu. When Three Charms But Four Alarms: Identifying the Optimal Number of Claims in Persuasion Settings. Available at SSRN: http://ssrn.com/abstract=2277117 or http://dx.doi.org/10.2139/ssrn.2277117
(3) University of Georgia. "Regular Exercise Plays A Consistent And Significant Role In Reducing Fatigue." ScienceDaily. ScienceDaily, 8 November 2006.
(4) Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 2007;107:1755–67. Search PubMed
(5) Journal of Science and Medicine in Sport 14 (2011) 4–9 Review. A review of the clinical evidence for exercise in osteoarthritis of the hip and knee Kim L. Bennell ∗, Rana S. Hinman
(6) Prim Care Companion J Clin Psychiatry. 2004; 6(3): 104–111. The Benefits of Exercise for the Clinically Depressed. Lynette L. Craft, Ph.D. and Frank M. Perna, Ed.D., Ph.D.
Oh my aching back! I must be turning 40.
What is it about getting close to 40 years of age? What was once a simple physical task with zero repercussions can quickly become a serious impediment to general movement for days (sometimes weeks and months) afterwards.
Elastics! You remember - “England, Ireland, Scotland, Wales - Inside, Outside, Inside, On!” Who knew this simple childhood activity could be fraught with danger for the nearly middle-aged. Earlier this year, on the rickety floorboards of our little house in Northcote, I decided to demonstrate to my children the art of elastics, only to find myself nursing a particularly sore low back, bum and leg once the demonstration had concluded. No, I didn’t trip on my ego, or anything 38-year old dad like that. I was just very sore afterwards. The muscles in my lower back and left bum cheek had well and truly gone into spasm. By the way, the Germans have a good phrase for acute low back pain - Hexenshuss (1). This literally means “shot by the witch”. I know I didn’t send my daughter to school at Hogwarts, so I safely ruled out the witch angle. The kids were actually impressed with my Quidditch like agility, until they saw me wince with pain.
The result of my brief foray into an innocent childhood activity resulted in three months of sciatica, or to use the correct terminology radicular pain, associated with inflammation or irritation of one of the nerve roots in my low back. I don’t have X-ray vision but I was pretty sure I had herniated one of my discs. While it definitely got me down, I sucked it up and chose to use this as a learning experience about my body and it’s ability to heal.
Acute low back pain with or without pain that heads into the bum or down the leg (radicular pain) is actually very common. Research dating to 1995 showed that low back pain was the 5th most common cause of visiting a GP (2). These numbers have only increased in the last decade. Most of you out there would think that having a disc herniation must mean bad things for the future? But some recent research debunks this entirely. Not only do you not need to have a disc herniation to experience sciatica, but results show that patients who DO have a disc herniation recover just as well from low back pain and sciatica as those who DO NOT have a disc herniation (3). WOAH!
Lets return to why this happened and what I did about it.
The why is actually not that clear. Doing an activity like elastics when you are 95kg as opposed to 22kg might have a lot to do with it. Aside from weight being a factor, we know from research that age does not necessarily predispose anyone to this happening. What we also know is that the more active, fit and conditioned an individual is when they tackle a physical task there is a decrease in likelihood of physical injury from performing that task. (4)
Well after three months I was back to my old self. The low back pain and sciatic symptoms improved with some osteopathic treatment, but mostly I took an active care approach involving graded exercise and pretty soon I was back to running the streets of Northcote with no pain at all.
I’ve found I do have to be a bit careful when doing something out of the ordinary but why that happens belongs in a totally other BLOG post.
Obviously not all back pain cases are created equal. For instance, when movement continually elicits pain then you might need to check in with your osteopath. It may be a more complicated clinical matter that needs addressing. But don’t worry in most case we can get you back on track and jumping elastics before you can say - Oh My Hexenshuss!
(1) Thanks Paul Ingraham for this little gem - saveyourself.ca
(2) Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Hart LG, Deyo RA, Cherkin DC. Spine (Phila Pa 1976). 1995 Jan 1;20(1):11-9.
(3) Magnetic resonance imaging in follow up assessment of sciatica. el Barzouhi A, Vleggeert-Lankamp CL, Lycklama à Nijeholt GJ, Van der Kallen BF, van den Hout WB, Jacobs WC, Koes BW, Peul WC; Leiden-The Hague Spine Intervention Prognostic Study Group. N Engl J Med. 2013 Mar 14;368(11):999-1007
(4) http://www.sciencedaily.com/releases/2009/02/090220090750.htm
Why Blog?
Navigating the manual therapy BS
As Osteopaths, we meet people like you who live with pain every day. We are passionate about how manual therapy can help relieve your pain. We are also passionate about the science of why you have pain, when it’s normal, why it’s there and how it got there. We know that we can educate you about pain, and in combination with some treatment you will live with less pain in your life. Don’t just take it from us, a study in 2003 showed that if you are educated about pain in combination with your therapy then you have better outcomes (1).
We’ve been procrastinating about blogging for several years. There is so much information out there. And we realised so much misinformation. Our aim is to write on topics informed by quality peer reviewed scientific literature.
There will be a mix of information on the blog. Much of it will be informed opinion, some of it educated speculation, and I’m sure at times it will be anecdotes about the body’s, maybe your body’s, amazing capacity for recovery.
1. Moseley, G. L. (2003b). Joining forces - combining cognition-targeted motor control training with group or individual pain physiology education: A successful treatment for chronic low back pain. Journal of Manual and Manipulative Therapeutics, 11, 88-94.
Stay tuned
We will be bringing you some interesting info on your body and how to look after it. Check back soon.